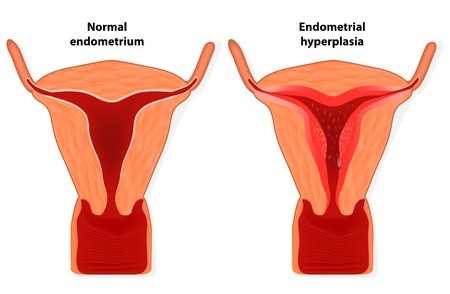
 Endometrial hyperplasia is a thickening of the uterine lining that can lead to bleeding and other symptoms.
Endometrial hyperplasia is a thickening of the uterine lining that can lead to bleeding and other symptoms.What is endometrial hyperplasia?
Endometrial hyperplasia is an overgrowth of the endometrium (uterine lining). The condition is most common in post-menopausal women and can lead to abnormal uterine bleeding. This overgrowth can increase a woman’s risk of developing endometrial cancer.
Causes of endometrial hyperplasia
Endometrial hyperplasia occurs when there is too much estrogen without progesterone. It is most often seen in women who are approaching, or who have completed, menopause and are experiencing irregular menstrual periods without ovulation. The estrogen over stimulates the lining of the uterus to grow and abnormal cell changes can also occur.
Endometrial hyperplasia is also associated with certain medications that act in a similar fashion to estrogen, long-term use of post-menopausal estrogen in women who have not had a hysterectomy, conditions that cause irregular menstrual periods and obesity.
Types of endometrial hyperplasia
Some types of endometrial hyperplasia carry a greater risk of developing endometrial cancer. Knowing your specific type of endometrial hyperplasia can help your gynecologist determine your risk of uterine cancer. There are 4 classifications of endometrial hyperplasia:
- Simple hyperplasia
- Complex hyperplasia
- Simple atypical hyperplasia
- Complex atypical hyperplasia
Atypical hyperplasia indicates abnormal cell changes have occurred and increases cancer risk.
Signs & symptoms of endometrial hyperplasia
Schedule an appointment with your OBGYN if you experience any of the following:
- Abnormal uterine bleeding –primary sign of endometrial hyperplasia
- Heavier or longer lasting menstrual periods – menstrual bleeding that deviates from your normal pattern
- Bleeding after menopause – any vaginal bleeding in post-menopausal women should be evaluated by a gynecologist
Diagnosing endometrial hyperplasia
A transvaginal ultrasound will allow your gynecologist to measure the thickness of the endometrial lining. If tissue samples are needed for microscopic examination, an endometrial biopsy, dilation and curettage (D&C) or hysteroscopy will be needed.
Treatment of endometrial hyperplasia
Progesterone may be prescribed by your OBGYN in shot or oral forms. The hormone may also be administered through the use of a vaginal cream or intrauterine device.
If atypical cells are present, hysterectomy may be recommended due to the increased risk of uterine cancer.
Lowering your risk of endometrial hyperplasia
Steps to help prevent endometrial hyperplasia include:
- Taking progesterone or progestin in combination with estrogen after menopause
- Oral contraceptives to regulate menstrual periods
- Losing weight if you are overweight